The QI Model for Clinical Peer Review
A Systems View of Peer Review
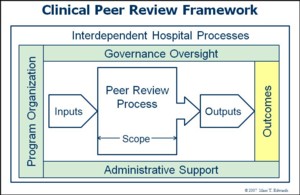
Since 2005, I've been looking for opportunities to improve this fundamental professional activity through the lens of a systems framework. In helping clients navigate multiple PDCA cycles, I've been refining a new model for clinical peer review process. I call it the QI Model to distinguish it from the prevailing QA Model, which has for so long limited the utility of peer review (see QA Model History).
The QI Model seeks to conduct peer review as a quality improvement activity, not only to improve the process itself, but to better align with the overall agenda of the organization to improve clinical performance and patient safety.
I applied this systems view in my work with Evan Benjamin on the first national study of peer review practices ever conducted in the US. We found that the key predictors of the likelihood that a program has significant ongoing impact on the quality and safety of care are the same as the key elements of the QI Model. In other words, the more that peer review looks like QI instead of QA, the more effective it is felt to be.
One important outgrowth of the 2007 survey was a 100-point, evidence-based 13-item Clinical Peer Review Program Self-Assessment Inventory. When applied to the original study population, the mean score was 45, suggesting huge opportunity for improvement across the country. No one scored at A-level, which may explain the dearth of examples of real success stories. These findings were validated and extended by the 2009 ACPE Clinical Peer Review Outcomes Study and the Longitudinal Clinical Peer Review Outcomes Study.
The QI Model continues to evolve. I added the key cultural differentiator of Trust based on the 2009 study results. At that time, I also added case identification via Self-Reporting based a recognition of the incongruity between a physician's Hippocratic obligation to "Do No Harm" and the sad reality that physicians are blocked from learning and sharing experiences of the unintended outcomes of care from fear of recrimination. This was later validated in the 2011-12 study. The most current free version of the Clinical Peer Review Program Self-Assessment Inventory derives from data collected in the 2015-16 update of the Longitudinal Clinical Peer Review Outcomes Study and reported in the International Journal for Quality in Health Care published Online First by Oxford University Press (April 9, 2018) doi:10.1093/intqhc/mzy069. It contains 20 items.
The QA and QI Models for Peer Review
The following table highlights the important differences between the QA and the QI Models for peer review.
| Aspect | QA Model | QI Model |
|---|---|---|
| Focus | Outliers | Shift the curve |
| Identify | Substandard care | Learning opportunity: system & individual |
| Determine | Competence | Performance |
| Inputs | Single case | Multiple cases |
| Case Finding | Generic screens | Self-reporting |
| Method | Judgment | Performance measurement |
| Process | Variable | Standardized |
| Reliability | Low | Good |
| Leverage Point | Expert opinion | Aggregate data |
| Orientation | Reactive | Proactive |
| Drivers | Fear, punishment | Trust, fairness, collegiality |
| Data Capture | "Leveling" against care standards | Multiple elements of performance |
| Relation to Hospital QI Process | Isolated | Highly interdependent |
| Accountability for Improvement | Low | High |
| Governance | Laissez faire | Attentive |
| Ultimate Process Outputs | Corrective action | System improvement Recognition of clinical excellence Performance feedback |
| ROI | Low | High |
| Net Effect | Culture of Blame | Culture of Safety |
Links
- The History of the QA Model
- Clinical Peer Review Process Improvement Resources
- Clinical Peer Review Program Self-Assessment Inventory
Research Agenda
Evidence-Based Answers
Whitepapers
Products & Services
- The Peer Review Enhancement ProgramSM
- PREP-MSTM: Program Management Software
- My PREPTM: Toolkit for Improvement
- Site Visit: A Jump-Start for Improvement