PREPSM Online Brochure
The Improvement Opportunity
Over the past decade, hospitals have come to embrace the Quality Improvement (QI) model that successfully transformed other industries. Through a variety of tools and techniques aimed at standardizing and improving processes, QI seeks to “shift the curve” towards higher performance (see Figure 1).
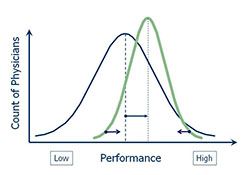
Figure 1: Quality Improvement
Clinical peer review, however, remains an anachronism. It is still commonly conducted within the Quality Assurance (QA) framework. By today’s standards, “Quality Assurance” was misnamed: it hasn’t assured either quality or patient safety. Neither has it served to eliminate substandard care. The QA model presumes that problems in care delivery can be minimized through inspection of untoward events to identify the underlying failure of professional judgment. As a result, peer review has been conducted with the primary objective of determining whether substandard care occurred and, if so, who was responsible - to prevent “the bad apples from spoiling the barrel.” This is tantamount to endorsing the false belief that simply trimming one tail of the distribution will substantially improve overall performance (see Figure 2). Thus, in many hospitals, peer review is rendered ineffective because it is threatening to individual careers and economic livelihood. It perpetuates a culture of blame and fails to promote a culture of safety.
In short, the QA model of peer review is fundamentally antithetical to our efforts to improve the overall quality of care. It is also wasteful. It captures only a small fraction of clinical performance data available to the review process. Moreover, it misses the opportunity to:
- Identify and correct problems in care processes and interfaces, which pose an ongoing threat to care quality and safety and which are 2-4 times as frequent as practitioner error
- Shift the curve of performance by providing timely and meaningful clinical performance feedback
- Leverage data from aggregate reporting and trend analysis iteratively improve both peer review process and clinical care
- Deal with the gray zone of performance below the threshold for adverse action, before a serious adverse event occurs, while the personal and organizational cost for correction is low
- Efficiently identify cases worthy of review by engaging physicians to self-report adverse events, near misses and hazardous conditions.
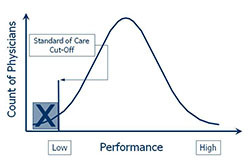
Figure 2: The Dysfunctional QA Model
Given all these limitations and inefficiencies of the QA model, the potential return on investment for improvement in peer review process is substantial.
The Solution
In the course of my client work and research, I have developed a useful alternative: From QA to QISM - The Peer Review Enhancement ProgramSM. PREPSM brings a quality improvement framework to clinical peer review. It takes any existing program and makes it better. It not only improves the process itself, but also engages the medical and nursing staff to conduct peer review the context of clinical performance measurement and improvement. PREPSM is readily implemented in an organization that has built consensus for change. When fully appreciated, the compelling logic of the program makes it easy to get agreement to proceed.
The basic prescription for the QI model includes these key ingredients:
- Distinguish between performance and competence
- View peer review as clinical performance measurement and improvement
- In each review, seek out whatever can be learned to improve both individual performance and the process of care
- Use contemporary case review methods to reliably measure clinical performance
- Standardize review committee processes
- Rationalize the connection with the hospital's performance improvement function
- Train reviewers, committee chairs and support staff
- Harness the power of information systems to aggregate data and analyze trends
- Provide timely and balanced performance feedback, including the recognition of excellence
- Track the outcomes of peer review
- Establish effective process governance and make ongoing improvements
- Keep the Trustees informed of the impact of peer review on quality and safety
- Promote self-reporting of adverse events, near misses and hazardous conditions under the protection of a Patient Safety Organization relationship
Case review forms, customized to fit the clinical activity prevailing in your organization, allow reviewers to readily rate multiple elements of performance having specific clinician attribution using reliable scales. This method generates 10-fold more clinical performance data with minimal additional effort. The added statistical power and scope of the data collected lowers the cost to assess variation and manage the program.
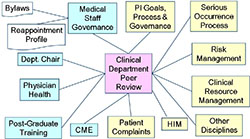
Figure 3: Interdependencies
Medical and nursing staff involvement is central to PREPSM. Involvement gets anchored in the activity of the advisory group which revisits the peer review process as embodied in policy. It grows through participation in review tool design whereby the various clinical specialties specify and validate their own relevant elements of care. It further expands during training and implementation. It comes to fruition when, without fear of reprisals, physicians and nurses are engaged to self-report cases knowing that the effort will contribute to improved quality and safety.
PREPSM exceeds Joint Commission standards, including focused and ongoing professional practice evaluation. It offers the added advantage of a vehicle by which physician and nurse leaders can take active ownership of an area of natural responsibility. Such action has currency with hospital management and can make a significant contribution to improved physician-hospital relations. In addition, with PREPSM, your organization is invited to participate in and benchmark against our normative database on peer review process and outcomes. You are also welcomed to join in our ongoing research agenda to publish studies on the impact of peer review process on the quality and safety of care and on other relevant outcome variables.
PREPSM is a partnership. You remain in control. In fact, without your involvement and leadership, the effort cannot succeed. PREPSM is a flexible framework that is customized to fit the complexities and nuances of your organization based on our initial discussions and preliminary assessment. The assessment need not be lengthy, but is important given the broad organizational interdependencies of the peer review process (see Figure 3).
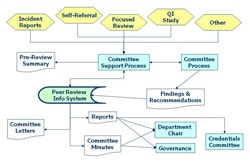
Figure 4: Enhanced Peer Review Process
The PREPSM methodology can accommodate simultaneous evaluation of post-graduate trainees as well as allied health professionals. PREPSM can also serve the needs of hospital systems and healthcare coalitions, especially when there is an interest in broadly standardizing tools and process.
PREPSM provides “straw man” templates to expedite the work of revising peer review policy, producing new review forms, and conducting reviewer training. Allowing for the schedules of the physicians who need to be involved in program design and for the organizational approval process for changes to peer review policy, PREPSM can be up and running in as little as three months.
I’ve also developed PREP-MSTM program management software to assure that you have the capability to fully implement the QI model. PREP-MSTM brings greater efficiency and effectiveness to both peer review support activity and process governance (see Figure 4). It extracts the actionable information from review data that will help you successfully drive clinical performance improvement. Physician and nurse peer review activity can be reported separately or combined. The license fee includes Patient Safety Organization reporting services and PREP-MSTM provides a simple mechanism for maintaining the related Patient Safety Evaluation System.
Through PREPSM, your program will become a source of pride as it more vigorously contributes to a culture of safety and quality. The peer review process will be well defined and transparent within the organization, and it will be primed for continued refinement.
Links
- PREPSM
- The QI Model
- The History of the QA Model
- Online Clinical Peer Review Program Self-Evaluation Tool
Whitepapers
Products & Services
- PREP-MSTM: Program Management Software
- My PREPTM: The Complete Toolkit for Program Improvement
- DataDriverSM: Accelerated Improvement
- From QA to QISM: Custom Solutions
- Client Testimonials
- Client Results