From QA to QI Volume 2 Number 3
Learning from Defects
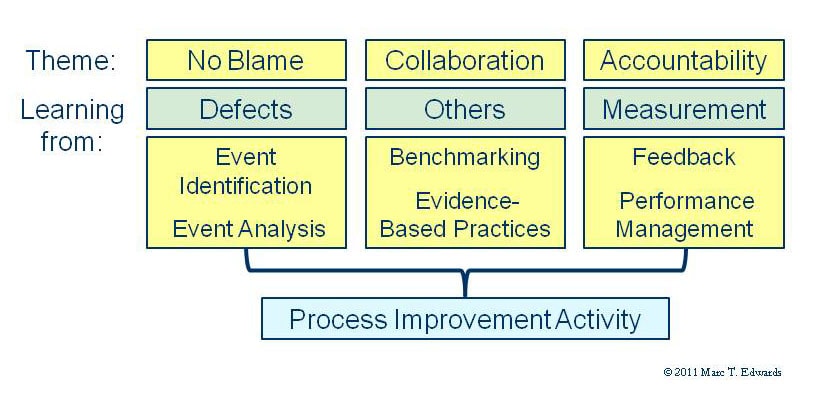
Now that we have gained a common vision of possibilities for a QI Model of peer review, it will be useful to return to our framework for improving patient safety to take a deeper dive into learning from defects.
Clinical peer review is the dominant mode of event analysis in US hospitals, but is not widely recognized as such. My 2007 study found that the median case review volume is 1-2% of hospital inpatient volume. This is more than an order of magnitude greater than the typical volume of formal root cause analyses (RCA). The problem is that the outmoded QA Model fails to generate organizational learning.
Case review volume is an element of the QI Model. Those of you who adhere to the principle that quality should be designed into a process in preference to inspection for defects might think this strange. The reality, however, is that healthcare is a poorly controlled process. Preventable adverse events run about 7% of admissions. Near misses and hazardous conditions are likely even more prevalent. If a hospital reviews only a small fraction of these, many opportunities for improvement will be missed.
Remember that the QI Model asks, “What can we learn from this case to improve clinical performance?” System and process issues are on the table along with handoffs and other issues of clinician to clinician communication/coordination. This vastly expands the return for the effort invested.
The causal analysis done during case review brings the experiences of all the review committee members into play – projected into the shoes of the responsible clinicians. It’s hindsight with empathy. It takes a little practice to start thinking more broadly about the factors influencing the outcomes of care, but it’s certainly not difficult. Once we get beyond the limitation of looking ONLY at clinical judgment, the door to real improvement opens. The conversation about judgment can still occur, but it needs to happen in the context of all potential contributing factors.
In a formal RCA, the exploration of potential contributing factors unfolds systematically. The exercise is time and resource intensive. In QI Model peer review, it’s much more abbreviated and intuitive. A search for strong interventions to prevent recurrence is required to get the desired payback. It helps if reviewers are given basic training in cause analysis so that they favor process improvement and forcing functions, over education and reminders. Graber has shown this is easy to do and has substantial benefit.
Peer review is certainly not the only option to expand the potential for learning from defects, but it does represent low hanging fruit ripe for picking. Some hospitals have adopted the Hopkins Comprehensive Unit-Based Safety Program (CUSP), whereby each nursing unit studies one problem each month and comes up with solutions. An added benefit of CUSP is that it teaches systems thinking to nurses and helps to balance the profession’s over-reliance on primary problem solving through workarounds. When many nursing units participate, the volume of learning from defects will fall somewhere between RCAs and peer review. Many staff will be engaged in the process and that’s a good thing for building a culture of safety.
If only we could solve the problem of efficiently identifying events, near misses and hazardous conditions that are worthy of analysis. We can. Stay tuned for my next column.
Coming Next: Self-reporting

Marc T. Edwards, MD, MBA
President & CEO
QA to QI
An AHRQ Listed Patient Safety Organization
References
- Graber ML. Physician participation in quality management: Expanding the goals of peer review to detect both practitioner and system error. Jt Comm J Qual Improv. 1999;25(8):396-407.
- Pronovost PJ, Berenholtz SM, Goeschel CA et al. Creating high reliability in health care organizations. Health Serv Res. 2006 Aug;41(4 Pt 2):1599-617. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1955341/?tool=pubmed
Links
- PSO Newsletter Index
- Clinical Peer Review Process Improvement Resources
- The History of the QA Model
- Ideal Clinical Peer Review Process Collaborative
- Normative Peer Review Database Project
Whitepapers
Products and Services
- The Peer Review Enhancement ProgramSM
- PREP-MSTM: Program Management Software
- My PREPTM: The Complete Toolkit for Improvement
- Medical Staff Opinion Survey
- DataDriverSM
- Client Testimonials
- Typical Client Results