A Framework for Patient Safety
Leverage Points for Improvement
This article does not reflect ongoing enhancements to the model. Please also refer to Removing Barriers to High Reliability. Full article available as PDF: Request Reprint
A makeover of this manuscript was accepted for publication in the American Journal of Medical Quality on 1/21/2016. It was published as: Edwards MT. An Organizational Learning Framework for Patient Safety. Am J Med Qual. February 25, 2016 doi:10.1177/1062860616632295 See the press release from 1/21/2016
Abstract
Despite the considerable efforts of healthcare organizations worldwide to improve patient safety, progress has been painfully slow. Although this likely reflects the difficulty of initiating and sustaining organizational change, it is complicated by a lack of conceptual models. This manuscript presents a framework for identifying leverage points for improvement and highlights several overlooked opportunities. The conceptual framework is structured around the fundamental modes of organizational learning. These include learning from others, learning from defects, and learning from measurement. They correspond with contemporary themes of collaboration, no blame for human error, and accountability for performance. The collaborative model of learning from others has dominated improvement efforts. Greater attention to the under-developed modes of organizational learning may foster more rapid progress in patient safety by increasing organizational capabilities, strengthening a culture of safety, and fixing more of the process problems that contribute to patient harm.
Background
Healthcare leaders worldwide have struggled to make measureable progress in patient safety. This likely reflects the overall difficulty of initiating and sustaining organizational change. Moreover, confusion abounds. For example, there is controversy regarding such basic issues as how to identify specific clinical practices suitable for widespread adoption (1, 2) and whether efforts should focus on medical injuries or errors (3, 4). More fundamentally, the confusion may signify faulty mental models for how to make progress. There is no conceptual framework available to guide leaders in identifying leverage points for improvement. As a result, most improvement efforts have copied successes in targeting specific patient subsets (e.g., those on ventilators or needing central line placement). Thus, much promising territory for improvement remains to be explored.
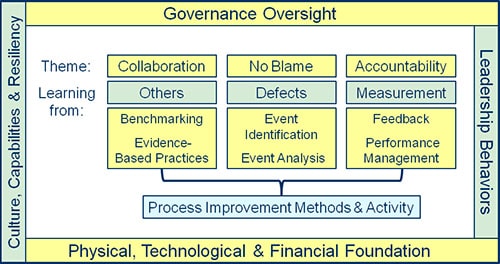
This paper presents a conceptual framework for patient safety built around the central task of organizational learning (see Figure). It is intended to make leverage points for improvement more visible. It emphasizes simplicity over comprehensiveness. Any such framework is unlikely to fully connect with the diverse perspectives and needs of all potential users. It can, however, serve as a useful starting point to stimulate further discussion and development.
Organizational learning is necessary to meet the challenges of improvement and transformative change. Such learning derives from 3 principal sources: the experiences of others as revealed in conversations and publications; the identification and analysis of process defects; and the use of process and outcomes measures to provide feedback and drive the organization’s performance management system. These 3 modes of learning correspond to major themes in the patient safety literature: collaboration, no blame for human error, and accountability for performance.
Each of the 3 modes of learning is important and worthy of enhancement. Improvement in any one need not be at the expense of any other. In particular, the belief that no blame must be balanced with accountability is misguided. It is not a matter of balance. In reality, we have achieved neither blame-free culture nor adequate accountability in healthcare. We need both along with collaborative learning from others.
Collaboration
Of these 3 modes of organizational learning, learning from others clearly dominates current practice. The multi-facility collaborative model has supported the most visible and successful work in patient safety. In addition, published literature has long been a rich source for improvement ideas and methods, enabling learning across organizations and national boundaries. Much value has also come to healthcare from study of other industries. In addition, normative databases are increasingly available as a means of benchmarking and best-practice identification.
Compared to initiating de novo work on organizational processes, it is generally easy to participate in a multi-facility collaborative or to extract ideas from published literature. The relative convenience of learning from others may have inadvertently contributed to the relative neglect of the other two modes of learning. It may also be that insufficient research effort has been applied to develop new content applicable to those modes.
For many, the greatest challenge related to collaborative learning is sustaining and spreading improvements across the organization. While the collaborative model has been invoked primarily to facilitate adoption of specific safety practices, it could also serve to advance best practices for learning from defects and measurement.
No Blame for Human Error
The principle of no blame for human error remains sacrosanct, but is difficult to uphold in day to day. Most organizations have been challenged to successfully hardwire a non-punitive response. For the past 5 years, it has consistently surfaced as the lowest scoring dimension in aggregate analysis of voluntarily submitted data from the Hospital Survey on Patient Safety Culture (5). Administrators consistently underestimate the extent to which the problem prevails.
Moreover, defects in the process of care are all too common and point to persistent weaknesses in event identification and analysis. This is unfortunate because systematic organizational learning from adverse events can improve safety (6, 7), and the results can be sustained over time (A. M. Wolff, personal communication). Roughly 7% of hospitalized Medicare patients in the USA suffer a preventable adverse event (8). Comparable rates have been reported in other countries. If one considers that serious latent process defects may also be associated with near-misses and no harm events, then the learning opportunity is even greater.
Typical event reporting systems identify only about 10% of adverse events (9). More robust, but inefficient and labor-intensive methods such as the IHI Global Trigger Tool are not a practical solution for routine event identification. On the other hand, where rapid response teams are in place, calls for help are easily identified and tracked. In this context, review of factors contributing to unexpected patient decline appears to offer fertile ground for improvement (10-12).
Even so, the relationship of weaknesses in event identification and analysis with the persistence of a blame culture has not been adequately appreciated. Another option to improve event identification goes to the heart of the matter. Clinicians invariably know when a patient suffers an adverse event, but are too often reluctant to report for fear of reprisal. Over the past 20 years, aviation successfully advanced passenger safety in large measure by developing policies and procedures to promote and protect self-reporting by pilots. The benefits of self-reporting have also been demonstrated in healthcare, but have not been widely adopted (13). The federal Patient Safety Act provides strong supports for self-reporting by simultaneously protecting the reporter from reprisals and the event analysis from discovery when conducted within a Patient Safety Evaluation System, as defined by the regulations (14). This requires a Patient Safety Organization relationship. Rapid growth in the number of listed Patient Safety Organizations over the past few years has made this option readily accessible.
Despite the recognition of deficiencies in the processes of event analysis and the availability of better models, little effort has been directed toward remediation. The effectiveness of root cause analysis, the resource-intensive mainstay of investigation for serious adverse events, has never been validated. As commonly practiced, the exercise tends to generate weak improvement recommendations, inconsistent implementation, and inadequate follow up to assure risk reduction (15, 16). A streamlined method of root cause analysis potentially applicable to a larger number of events has been described, but there is as yet no data on its rate of use or effectiveness (17).
Clinical peer review is the other important approach to event analysis. It is broadly and frequently applied in hospitals world-wide among physicians. It may also be used by other disciplines. In contrast to root cause analysis of serious events, it consumes few resources (18). Although the dominant quality assurance model that seeks to “keep the bad apples from spoiling the barrel” perpetuates a toxic culture of blame and fails to contribute to improved safety, a more effective quality improvement model has emerged that warrants leadership attention (19). Model factors include standardization of process, recognition of excellence, attentive program governance, integration with other hospital performance improvement activity, reviewer participation, and identification of clinician to clinician issues (as well as other process problems) during the review process. The shift required to improve the peer review process is small compared to the task of scaling up some novel method of event analysis. Fundamentally, it is as simple as changing the primary question of the case review process from “Is there evidence of substandard care?” to “What can we learn from this case to improve clinical performance?” Thus, clinical peer review remains the most promising vehicle to efficiently extract the largest number of learning opportunities from the diverse array of clinical scenarios prevalent in each unique healthcare organization.
Accountability for Clinical Performance
Healthcare organizations have also struggled to improve clinical performance by learning from measurement, most visibly in relation to unprofessional behaviors (20) and non-compliance with widely accepted safety-related practices (21). Although blatantly reckless disregard for patient safety is thankfully rare among healthcare professionals and staff workers, it mandates prompt intervention whenever it occurs. Much more problematic is the grey zone characterized by unconscious drift into risky choices conditioned by normalization of deviance, conflicting situational factors, and the need to workaround problematic processes. This calls for correction of poorly designed processes, strategies to bring awareness to drift, and targeted management action to rein in habitual deviation.
The Joint Commission standards promulgated in 2008 that mandated focused initial and ongoing professional practice evaluation to supplement the bi-annual credentialing process have spurred efforts to better measure clinical performance. The common approach has been to rely on whatever can be extracted from administrative systems. The resulting measures have been more meaningful for evaluating procedural activity than cognitive performance. This need not be the case. Performance measurement encompasses the subjective evaluations made by peers and managers, as well as the explicit data captured by information systems and manual abstraction. Robust methods for making subjective performance measurements are available (22). If we did a better job of linking performance measurement, data management and feedback, we might be more successful at promoting self-correcting behaviors and, thereby, reduce the need for the more difficult performance management conversations.
Process Improvement
The 3 modes of learning converge to impact patient safety through the final common pathway of process improvement, whether at the organizational, micro-system or individual work-habits level. Healthcare organizations have gained increasing fluency and sophistication with process improvement methods over the past decade. This includes organizational-level coordination, support, management and oversight of improvement activity. Even so, implementation of process change remains a challenge.
When considering individuals, we think of processes as habits. Changing personal habits and routines requires sustained attention and some degree of effort. There is growing appreciation that this requirement is based in the biology of the human nervous system. Insofar as all organizational change requires some members to adopt new habits and insofar as most efforts at major organizational change fail throughout the business world, of necessity, our understanding of how to promote and support such change must continue to evolve. In this context, the painfully slow improvement in patient safety is understandable, but not condonable.
Inter-Relationships
In order to preserve clarity, the graphical presentation of the conceptual framework omits the inter-relationships between the various elements. These inter-connections suggest potential for synergistic improvements. For example, clinical performance measurements can be made during event analysis as has been demonstrated for peer review (23). Such measures could be efficiently captured and used to increase accountability through feedback and performance management, without compromising the principle of no blame for human error.
Organizational Framing Factors
The conceptual model sets the 3 modes of learning within a 4-sided frame of governance oversight; leadership behaviors; the physical, technological and financial environment; and organizational culture, capabilities and resilience. Each of these framing factors is inter-dependent with the other elements of the model and may themselves be leverage points for improvement in patient safety. For example, even though the trustees carry ultimate responsibility for organizational performance, effective governance activity also needs to occur at other levels.
The framework intentionally emphasizes process over structure. Form should follow function. Structure can be considered to fall within the purview of governance and leadership. Since organizational structure should logically support strategy, safety will not be the only driver. In any case, the hierarchical command and control model of organizational design is ill-suited to produce the learning and the flexibility required for rapid change.
Many think of leadership in terms of formal authority, but practically speaking, leadership is a verb. Anyone in the organization, regardless of role, can exhibit leadership behavior that contributes to improved safety. It is most desirable that front line workers should be so engaged. Conversely, the titled leaders of the organizational hierarchy may lack the training and skill to function effectively in their roles. Such deficiency can greatly constrain organizational capabilities and obstruct progress. This problem may be more common in healthcare than in other industries, especially among clinicians who acquire management responsibilities. If the key task of a learning organization is to develop improved thinking at all levels, leaders must play a critical enabling role through their daily interactions for such improvement to occur (24). Development of strong, deep leadership has potential to catalyze improvement in performance (25).
The inadequacies of performance management processes highlighted above stem from deficiencies in leadership behaviors. Nowhere is this more evident than in the normalization of deviance. This is doubly problematic because it allows unsafe habits to be established that are difficult to change. In addressing these problems, leaders must use caution in their choice of models and language. In particular, “justice” and “punishment” make good sense in court of law, but do not evoke healthy emotions when applied to safety culture in healthcare. “Fairness”, “accountability”, and “respect” might be better choices. Algorithms to evaluate “blame-worthy” acts will inevitably be misapplied by frontline managers with serious unintended consequences for the organization.
Physical plant, technology and finances are the more tangible aspects of the infrastructure that potentially impact patient safety among hospitals worldwide. Financial challenges are increasingly common and can limit the capacity to invest in technology and update the physical environment using evidence-based design. Still, the greatest danger may be in viewing technological or structural investments as a panacea. Notwithstanding financial constraints, they carry a prolonged time line for implementation. People and process remain the most critical and malleable components of the system of care.
Much has been written about organizational culture. While its limiting effects are pervasive, the good news is that every successful patient safety initiative helps to advance a culture of safety and build capabilities. Given the high rate of adverse events and medical error, the importance of resilience to recover from failure at both the personal and organizational level has been increasingly recognized. This creates a potential nurturing role for leadership which integrates nicely with the need to practice mindfulness in order to retrain the gut responses which spontaneously cast blame for human error.
Conclusions
The conceptual framework herein described may be of value in helping healthcare leaders identify the most promising leverage points for improvement in their respective organizations. Opportunities abound. Most will derive benefit by adopting improved methodologies for event identification, event analysis, and performance management. Greater attention to these under-developed modes of organizational learning may foster more rapid progress in patient safety by increasing organizational capabilities, strengthening a culture of safety, and fixing more of the process problems that to contribute to patient harm.
Acknowledgments
The author gratefully acknowledges critical reviews of the draft manuscript by Larry Tonberg Edwards, PsyD, Dennis Ehrich, MD, Azita Hamedani, MD, MPH, and Robert Klugman, MD.
Biographical Sketch
The author is the President and CEO of QA to QI, West Hartford, CT. He applies 25 years of healthcare management and consulting experience to run a federally-listed Patient Safety Organization, conduct studies in health care operations improvement, and assist hospitals to improve quality, patient safety and resource management.
References
- Leape LL, Berwick DM, Bates DW. What practices will most improve patient safety? Evidence-based medicine meets patient safety. JAMA. 2002;28(4):501-507.
- Shojania KG, Duncan BW, McDonald KM, et al. Safe but sound: patient safety meets evidence-based medicine. JAMA. 2002;28(4):508-512.
- Layde PM, Maas LA, Teret SP, et al. Patient safety efforts should focus on medical injuries. JAMA. 202;287(15):1993-1997.
- McNutt RA, Abrams R, Aron DC. Patient safety efforts should focus on medical error. JAMA. 202;287(15):1997-2001.
- Hospital Survey on Patient Safety Culture. March 2011. Agency for Healthcare Research and Quality, Rockville, MD. http://www.ahrq.gov/qual/patientsafetyculture/hospsurvindex.htm (accessed 25 July 2011).
- Wolff AM, Bourke J, Campbell IA, Leembruggen DW. Detecting and reducing hospital adverse events: outcomes of the Wimmera clinical risk management program. Med J Aust. 2001;174(12):621-5.
- Wolff AM, Bourke J. Detecting and reducing adverse events in an Australian rural base hospital emergency department using medical record screening and review. Emerg Med J. 2002;19(1):35-40.
- Office of Inspector General. Adverse Events in Hospitals: National Incidence among Medicare Beneficiaries. OEI-06-09-00090. November 2010. http://oig.hhs.gov/oei/reports/oei-06-09-00090.pdf (accessed 25 July 2011).
- Office of Inspector General. Adverse Events in Hospitals: Methods for Identifying Events. OEI-06-08-00221. March 2010. http://oig.hhs.gov/oei/reports/oei-06-08-00221.pdf (accessed 25 July 2011).
- Kaplan LJ, Maerz LL, Schuster K, et al. Uncovering system errors using a rapid response team: cross-coverage caught in the crossfire. J Trauma 2009;67(1):173-178.
- Braithwaite RS, DeVita MA, Mahidhara R, Simmons RL, Stuart S, Foraida M: Use of medical emergency team (MET) responses to detect medical errors. Qual Saf Health Care 2004, 13:255-259.
- Iyengar A, Baxter A, Forster AJ: Using Medical Emergency Teams to detect preventable adverse events. Crit Care. 2009; 13:R126-R130. http://ccforum.biomedcentral.com/articles/10.1186/cc7983.
- Katz RI, Lagasse RS. Factors influencing the reporting of adverse perioperative outcomes to a quality management program. Anesth Analg. 2000;90:344–350.
- Edwards MT. Engaging physicians in patient safety through self-reporting of adverse events and better clinical peer review process. Phys Exec. 2012 (in press).
- Percapio KB, Watts BV, Weeks WB. The effectiveness of root cause analysis: what does the literature tell us? Jt Comm J Qual Patient Saf. 2008;34(7):391-398. 22.
- Wu AW, Lipshutz AKM, Pronovost PJ. Effectiveness and efficiency of root cause analysis in medicine. JAMA. 2008;299(6):685-687.
- Pronovost PJ, Holzmueller CG, Martinez E, et al. A practical tool to learn from defects in patient care. Jt Comm J Qual Patient Saf. 2006;32(2):102-108.
- Edwards MT, Benjamin EM. The process of peer review in US hospitals. J Clin Outcomes Manage. 2009(Oct);16(10):461-467.
- Edwards MT. The Objective Impact of Clinical Peer Review on Quality of Care. Am J Med Qual. 2011;26(2):110-119. http://ajm.sagepub.com/content/26/2/110.short.
- Hickson GB, Pickert JW, Webb LE, Gabbe SG. A complementary approach to promoting professionalism: identifying, measuring, and addressing unprofessional behaviors. Acad Med. 2007;82(11):1040-1048.
- Wachter RM, Pronovost PJ. Balancing “No Blame” with Accountability in Patient Safety. NEJM. 2009;316(14):1401-1406.
- Streiner DL, Norman GR. Health Measurement Scales: A Practical Guide to their Development and Use. 3rd ed. New York, NY: Oxford University Press; 2003.
- Edwards MT. Measuring clinical performance. Phys Exec. 2009;35(6):40-43.
- Rock D. Quiet Leadership: Six Steps to Transforming Performance at Work. New York, NY: HarperCollins 2006.
- Walsh KE, Ettinger WH, Klugman RA. Physician quality officer: a new model for engaging physicians in quality improvement. Am J Med Qual. 2009 Jul-Aug;24(4):295-301.
Links
- Clinical Peer Review Process Improvement Resources
- The QI Model for Clinical Peer Review
- The History of the QA Model
- Ideal Clinical Peer Review Process Collaborative
- Normative Peer Review Database Project
Whitepapers
Products and Services
- The Peer Review Enhancement ProgramSM
- PREP-MSTM: Program Management Software
- My PREPTM: The Complete Toolkit for Improvement
- DataDriverSM
- Client Testimonials
- Typical Client Results